Patients rarely tell you that the noise of their concentrator is bothering them.
They’ll mention poor sleep. Feeling “on edge.” Not wanting the machine in the room with them. Some will quietly reduce their usage because the constant hum becomes too much.
For many people on oxygen therapy, noise isn’t a small annoyance, it’s an everyday barrier to comfort, rest, and adherence.
The aim of this guide is simple: give clinicians a set of practical, evidence-informed tips you can share with patients to help them create a quieter, more comfortable home environment.
Why Concentrators Make Noise. A Quick Explainer for Patients
Helping patients understand why their machine makes noise can reduce frustration and improve confidence in using it.
Fans
Patients may notice a light hum. If the fan is working harder (dusty filters or limited airflow), this hum gets louder.
Compressor
Most of the “steady background noise” comes from here. Patients often describe it as a purr, throb, or low drone.
Blocked vents or filters
Restricted airflow increases sound, much like breathing through a narrow straw.
Vibrations
Loose screws or a hard surface underneath the device can turn soft noise into a rattling or buzzing tone.
A short, simple explanation often helps patients feel more in control and less anxious about the sound their device makes.
Clinician Note: When a Quiet Device Makes the Biggest Difference
For some patients, especially those with:
-
insomnia or light sleep
-
anxiety or sensory sensitivity
-
small or shared living spaces
-
24-hour therapy requirements
…the noise burden adds up.
The Kingon P2-E is currently one of the quieter portable concentrators available in Australia. Its reduced vibration, gentle fan modulation, and compact build make it easier for patients to use the device near family areas or overnight with minimal interruption.
This is not a sales pitch, but a quiet concentrator can genuinely influence adherence and wellbeing, and the P2-E is often the model clinicians recommend when noise sensitivity is an issue.
Practical Noise-Reduction Strategies You Can Teach Patients
These suggestions are simple, low-risk, and easy for patients to follow.
1. Help Patients Choose the Right Location
Sometimes the loudest part isn’t the machine, it’s where it’s sitting.
Placement tips you can share:
- Move the device slightly away from the bed or TV chair. Even a metre or two makes a big difference.
-
Soft furnishings (rugs, curtains, fabric lounges) absorb noise.
-
Hard surfaces (tiles, benchtops, timber floors) amplify vibration.
-
Never place the device inside a closed cupboard. Restricted airflow forces the fan to work harder and increases sound.
A quick conversation about placement often gives patients an immediate improvement at home.
2. Encourage a Simple Maintenance Routine
Most patients don’t realise how much louder their device becomes when filters and vents aren’t cleaned regularly.
Key reminders:
-
Clean or replace filters as per manufacturer guidelines.
-
Wipe dust away from vents and surrounding areas.
-
Check for loose screws or rattling panels.
-
Report any sudden change in noise, pitch, or rhythm.
Patients who understand this tend to maintain their equipment better. Reducing both noise and mechanical strain.
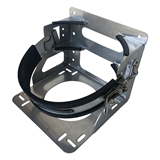
3. Reduce Vibration at the Source
You can explain this with a simple analogy:
“Imagine placing a phone on a desk versus a cushion. One vibrates loudly, the other barely makes a sound.”
Practical tips:
-
An anti-vibration mat under the concentrator reduces rattling.
-
Avoid thin tables or bench-tops that echo or amplify sound.
-
Make sure padding doesn’t block airflow.
Vibration dampening is one of the easiest wins for noise-sensitive patients.
4. Consider Noise-Dampening Accessories
There are purpose-built covers and enclosures designed to soften the mechanical noise of concentrators.
The key message to relay:
If patients use covers, they must be medically appropriate and allow full ventilation.
Anything that traps heat is unsafe.
5. When a Quieter Model Is Clinically Helpful
In some cases, the noise burden itself becomes a barrier to therapy. That’s the moment to explore quieter devices.
Clinicians can guide patients to look for:
-
decibel ratings under ~40 dB
-
smoother compressor mechanics
-
efficient cooling systems
-
patient reviews mentioning low noise
Portable concentrators (like the Kingon P2-E) often deliver lower noise profiles than larger stationary units.
Additional Tips Clinicians Can Suggest
These aren’t medical interventions, they’re simple lifestyle supports that help patients cope with sound during therapy.
White noise machines
Useful for masking the hum at night.
Comfortable earplugs
Helpful for light sleepers, provided oxygen delivery isn’t compromised.
Regular check-ins
Asking “How are you going with the sound of your concentrator?” opens up space for honest discussion.
Collaborative troubleshooting
Sometimes clinicians discover that patients are using the device in a setting that unintentionally increases noise - a kitchen bench, a hollow table, or a tight corner.
A quick adjustment often resolves it.
Key Clinical Takeaways
-
Noise is a genuine quality-of-life issue for many oxygen therapy patients.
-
A few environmental changes can significantly reduce perceived loudness.
-
Good maintenance reduces mechanical noise and supports device longevity.
-
Anti-vibration strategies are inexpensive and effective.
-
When noise becomes a barrier to adherence, moving to a quieter model (such as the Kingon P2-E) can be clinically justified.
-
A quiet environment supports better sleep, reduced stress, and higher compliance.
Closing Note for Clinicians
Patients often assume the noise is “just part of it” and suffer in silence.
By raising the topic proactively and offering a few simple strategies, you can help them create a calmer, more comfortable therapy routine, and in many cases, improve their long-term outcomes.

















-205x205.jpg)


-205x205.jpg)
Large-205x205.jpg)













